Veterans Care Today: Dr. Kenneth Campbell Of Tulane University On How The US Has Improved Its Care For Veterans Over The Past Five Years
An Interview With Eric Pines
Be very patient, enjoy each day and plan better.
The daily headlines remind us of how countries around the world care or do not care for their military service members. How does the United States hold up with regard to how it cares for its veterans? We know in the past questions have been raised about the VA system, but it seems that a corner has been turned and veterans’ care has improved. How exactly has the VA system been improved? How does the US care for veterans compared to other comparable countries? What exciting new technological or methodological innovations are being used to improve veterans’ health outcomes? To address these questions, we are talking to successful physicians, healthcare workers, veterans, or other VA employees and officials who can share stories and insights from their experience about the state of veterans’ care today and how the US has improved its care for veterans over the last five years.
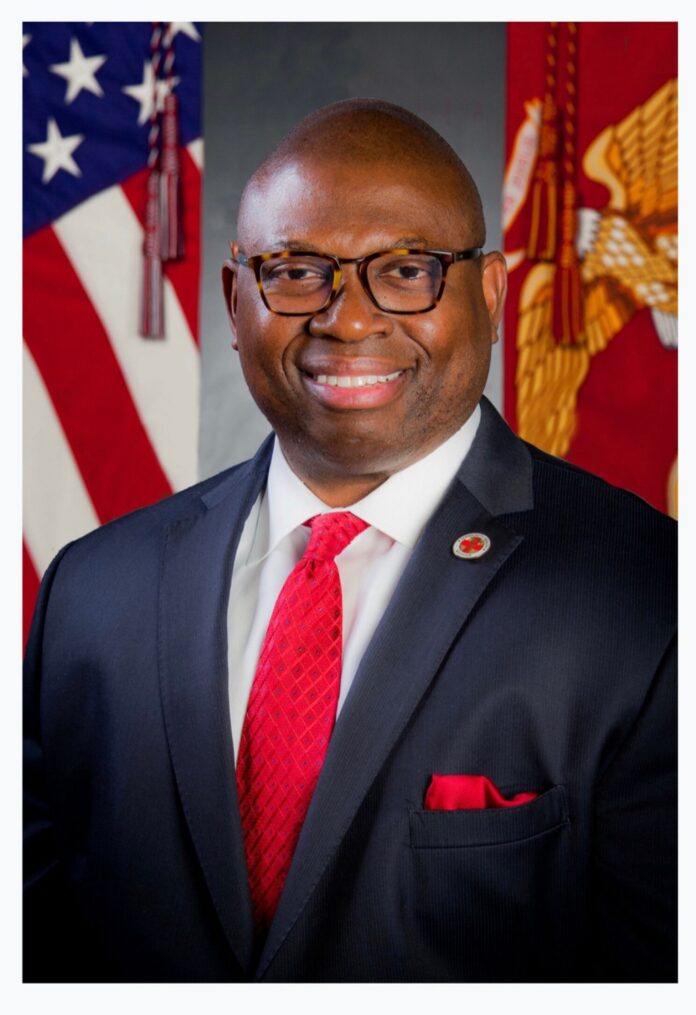
As a part of this series, I had the pleasure to interview Dr. Kenneth Campbell.
Dr. Kenneth Campbell, DBE, MPH, MBA, MA, is the Director of the Tulane University Master of Health Administration Online Program and Clinical Assistant Professor, in the Tulane University Department of Health Policy and Management.
Thank you so much for joining us in this interview series! Before we dive into our interview, our readers would like to get to know you a bit. Can you tell us a bit about your backstory and a bit about what brought you to this specific career path?
I am Dr. Kenneth Campbell, DBE, MPH, MBA, MA, Director of the Tulane University Master of Health Administration Online Program and Clinical Assistant Professor, in the Tulane University Department of Health Policy and Management.
I am also an American veteran who served in the United States Marine Corps for six years and served in operations Desert Storm and Desert Shield. For my service and dedication, I earned the Good Conduct Medal, Letter of Appreciation, Meritorious Mast and the National Defense Service Medal. My tour in the Marine Corps provided a foundation of values and leadership skills that have taught me about ethics in leadership, the philosophy of leading by example, and the importance of teamwork.
As a decorated Marine in the field of financial management during Desert Storm and Desert Shield, I provided financial support under the Commanding Officer of Financial Disbursing where I was responsible for millions of dollars in financial transactions. This included military pay, adjustments, advances, taxes and other special payments assignments that were being performed daily for Marines and their families. I oversaw the operations, development and implementation of millions of dollars in financial military projects consisting of hardware and software deployment for financial management processing of Marine divisions and HQHQRON MCAS squadrons on the base and in the field of military training.
Following my military service, I earned both a Biology (with a biochemistry focus) and Experimental Psychology (with a African American History focus) Bachelor’s Degree from the University of South Carolina. After my graduation, I had the unique opportunity to work in Cardiology for a year studying left ventricular dysfunction (LVD) in congestive heart failure (CHF) in veteran patients who suffered from heart problems. In 2006, I earned both a Master’s in Public Health (MPH) and a Master’s in Business Administration (MBA) from Benedictine University plus several certifications in the areas of Managed Care, Long Term Care and Health Care Administration. I was trained in Lean Six Sigma in healthcare at Loyola University and earned my third degree of Master of Art (MA) in Bioethics and Health Policy in addition to a Doctorate Degree in Organizational Ethics and Health Policy (DBe) from Loyola University, Stritch School of Medicine/Neiswanger Institute for Bioethics in Chicago, Illinois.
Having a love and affinity for education and leadership, I later completed a Certificate in Leadership Strategies For Evolving Healthcare Executives at the Harvard University School of Public Health, along with a continuing professional education fellowship in “Driving Business Performance: Culture of Health Care Executive Leaders.”
I grew up in a very rural area in the South and I will never forget the heroism of the doctors and nurses at the local hospital (which is permanently closed today) in the emergency room department. They surgically placed my heel back on my foot when it was 95% cut off and hanging on only by the thin skin that remained.
One night, I was playing with friends in some thick vegetation which included a lot of bushes and trees. What I was unaware of, was the sharpness of the roots around the base of the trees. To make a long story short, I was not looking where I was placing my feet as I ran through the bushes playing hide-and-seek. I stepped on a sharp root sticking up and it sliced off the heel of my foot. Arriving at the emergency room, I prayed for the best but could not accept the worst- that I would never walk or run like I used to. These angels of healthcare workers, the doctors and nurses, began to work on me in no time. I was in pain and never felt anything like it in my life but my prognosis after they were done was better than I could hope for. Within months, I was back-up and running and playing like nothing ever happened.
So, what brought me into this specific field was to ensure that my hospital, healthcare organization or health system has everything it needs to aid in the heroism of doctors, nurses, and other healthcare professionals. I wanted to make sure they have what they need to help provide miracles to the next patient that comes through that door for medical and preventive services regardless of their race, ethnicity, age, ability to pay or immigrant status. I just see people, not economic status — just people that are in need of help and we have to help them.
Can you share the most interesting story that happened to you since you began your career?
I do not know if I have just one interesting story. But I would say for me it was the experience I witnessed working in rural and urban communities and seeing the impact of racism and the factors that affect children and adolescent health. This leaves a large percentage of children more vulnerable to poor health and poor outcomes which were preventable. When you look at health disparities, health inequities and mental health problems in children and adolescents, racism is the social determinant of health that has the potential of impacting millions of children’s health and health inequities. When I was an undergraduate at the University of South Carolina, I was blessed to meet this very wise pediatrician who shared a common interest in seeing more pediatric care available to black and brown communities where it was largely lacking despite having hospitals around. It was rationalized at that time that one in every four patients was at the federal poverty level (FPL). Knowing pediatricians with private practices at that time had a unique opportunity to discuss with families of all races the importance of getting high-quality care and having access in a system that put up obstacles that prevented them from getting the care needed at an affordable price, this pediatrician decided to build such building so those who were below the poverty level or had trust issues with healthcare could get care from minority pediatrician. However, it took a lot of funding to lift this dream and therein lies the problem. Traditional financial institutions, hospitals, and health systems all turned him down. For many of these sources, their perspective was that this pie in the sky dream was the equivalent of pouring good money into a bucket with a large hole in the bottom, and the return on investment was too risky. This pediatrician believed in optimizing systems and leveraging the location of this clinic to provide year-round, accessible, high-quality, and compassionate care to the poor. So, he turned to the NFL and one of my favorite NFL heroes of the game made this clinic possible by financing the building of the great clinic that stands today in Columbia, South Carolina. My story is this: if one man’s dream of eradicating racism in healthcare and putting people first, can result in more than 80 highly qualified providers delivering integrated healthcare services to more than 61,000 individuals annually, I can do the same as a future CEO of a healthcare system or hospital.
Can you please give us your favorite “Life Lesson Quote”? Can you share how that was relevant to you in your life?
A quote by Martin Luther King Jr and his quote on Equality Rights-
“If a man has not discovered something that he will die for, he isn’t fit to live.”
For me, that something has been joining the Marines and being on this academic journey of excellence to be great at operating, and optimizing my own healthcare system one day through community engagement, advocacy and public policy so that no human being goes without healthcare services in any community.
Are you working on any exciting new projects now? How do you think that will help people?
During the pandemic, I had the unique opportunity thanks to my boss at the time, Dr. Ezike, the Director of Illinois Department of Public Health (IDPH) to oversee the mass logistics and operation of our Mass Vaccination and Testing sites through the state of Illinois. In addition, I helped lead our Illinois National Guards (rural and hard to reach areas) and traveling nurses, doctors, contracted providers and other healthcare professionals into communities to provide vaccination all over the State of Illinois regardless of location. Thanks to our Governor, accessibility was not an issue and Illinois’s rate of vaccination was very high.
Now, I am working with my colleagues on the first state certification and reimbursement program for Community Health Workers (CHWs) in Illinois. I believe that community health workers can contribute to improved behavioral and health outcomes and reductions in health disparities. Having worked in healthcare for over 20 years, and seeing the workforce shortage that is occurring, I predict CHWs will be an extension of providers to deliver community interventions to meet differing needs and populations across communities. They will bridge the gap between health care services and community members, build community and individual capacity to plan and implement interventions addressing multiple chronic health conditions, and meet community needs in a culturally appropriate manner.
How would you define an “excellent healthcare provider”?
An excellent healthcare provider in my eyes is someone who is compassionate; treating others (patients and their families) with respect and dignity. They are fair and take time to explain and educate the patient and their families on the care they are seeking and the services that are being provided. They are someone who improves individual, community and population health and provides access to all. Someone who focuses on healthcare outcomes and believes in using data, best practices and evidence-based approaches to deal with complex healthcare problems in a complex healthcare environment.
Ok, thank you for that. Let’s now jump to the main focus of our interview. Based on your experience can you please share three recent improvements to veterans care that you are really pleased about?
First, the PACT Act (Promise to Address Comprehensive Toxics) marks the most significant expansion of VA health care in 30 years. When our soldiers go to war and off to foreign lands to fight for this country, they are being put in high-risk areas that increase health risk. From chronic diseases like cancers, asthma, heart disease, lung disease and so much more like PTSD, we have to take care of our veterans better. I am also thankful as a veteran for the bravery and fight of so many families for their veterans, and a special thanks from my heart goes out to comedian Jon Stewart who took it to Washington and fought for “US.” This legislation removes the need for certain veterans and their survivors to prove service connection if they are diagnosed with one of 23 specific conditions.
The second improvement was the American Jobs Plan Supports Veterans policy. The American Jobs Plan would help meet the needs of veterans by creating millions of good jobs for veterans and their spouses, growing opportunities for small-veteran-owned business, and helping ensure the delivery of world-class, state-of-the art health care throughout the Department of Veterans Affairs.
The last thing I would say is the improvement of State policies for women veterans. Today, women makes-up around 20% of new recruits, 15% active duty and 18% of the guard and reserve forces. On December 3, 2015, the Defense Secretary Ashton Carter announced that the Pentagon would open all combat jobs to women with no exception. That is a great thing!
In contrast, can you highlight three areas of veterans care that still need improvement? What would you suggest needs to be done to address those challenges?
IT, Quality and Staffing, just to name a few.
Information Technology:
I think the department needs to update its EMR, its VA loan electronic reporting interface and just its clinical systems in general. Based on what I have read, about 75% of the department’s IT budget goes toward maintaining old VA systems. Certainly, moving more into the AWS or using newer EMRs would vastly improve data collections, improve Veterans health outcomes and be more informative and data sharing among health care professionals (between primary and specialist) who are directly involved with the patient’s care.
Quality:
Wait-time improvements and quality data metrics need to occur for our Veterans. Each VA facility needs a quality improvement team of 12 people whose sole function is to improve quality continuously in every area of the facility. For example, adopting specialized teams and performance improvement plans.
Staffing:
For most VA organizations, the hiring process needs improving. The department must be able to fill vacancies in 6 months or less. As mentioned before, their IT infrastructure for human resources needs to be updated. In the long run this will provide what positions are available so the right people can get hired. Another area that needs improvement is in the payment scale of its employees. The VA payment scale for their employees needs to be aligned with the private sector. This will keep people in jobs longer and they will not have to deal with the labor shortages.
From your perspective how does the US care for veterans compared to other comparable countries?
I think the US’s care for veterans compared to other comparable countries is excellent. Sure we have some quality improvement issues to work out, but the US VA system is a good system for veterans of the old and new.
This is our signature question that we ask in many of our interviews. What are your “5 Things I Wish Someone Told Me When I First Started My Career”?
- How rewarding health administration can be and the impact policy has on populations’ access to healthcare.
- How challenging health disparities, health literacy, justice and social determinants of health are associated with life expectancy.
- How important science and viruses were to our survival and longevity.
- The importance of relationships, networking and the value of teams in healthcare.
- Be very patient, enjoy each day and plan better.
You are a person of great influence. If you could inspire a movement that would bring the most amount of good to the most amount of people, what would that be? You never know what your idea can trigger. 🙂
I would continue to encourage our youth to be agents of change. People who are willing to put in the work, tackle head on the challenges and injustices of today and tomorrow. Finally, to love and have compassion for one another. But most of all, be kinder to each other.
How can our readers further follow your work online?
Your followers can follow me on my LinkedIn
Thank you so much for these insights! This was very inspirational and we wish you continued success in your great work.
About the Interviewer: Eric L. Pines is a nationally recognized federal employment lawyer, mediator, and attorney business coach. He represents federal employees and acts as in-house counsel for over fifty thousand federal employees through his work as a federal employee labor union representative. A formal federal employee himself, Mr. Pines began his federal employment law career as in-house counsel for AFGE Local 1923 which is in Social Security Administration’s headquarters and is the largest federal union local in the world. He presently serves as AFGE 1923’s Chief Counsel as well as in-house counsel for all FEMA bargaining unit employees and numerous Department of Defense and Veteran Affairs unions.
While he and his firm specialize in representing federal employees from all federal agencies and in reference to virtually all federal employee matters, his firm has placed special attention on representing Veteran Affairs doctors and nurses hired under the authority of Title. He and his firm have a particular passion in representing disabled federal employees with their requests for medical and religious reasonable accommodations when those accommodations are warranted under the Rehabilitation Act of 1973 (ADA). He also represents them with their requests for Federal Employee Disability Retirement (OPM) when an accommodation would not be possible.
Mr. Pines has also served as a mediator for numerous federal agencies including serving a year as the Library of Congress’ in-house EEO Mediator. He has also served as an expert witness in federal court for federal employee matters. He has also worked as an EEO technical writer drafting hundreds of Final Agency Decisions for the federal sector.
Mr. Pines’ firm is headquartered in Houston, Texas and has offices in Baltimore, Maryland and Atlanta, Georgia. His first passion is his wife and five children. He plays classical and rock guitar and enjoys playing ice hockey, running, and biking. Please visit his websites at www.pinesfederal.com and www.toughinjurylawyers.com. He can also be reached at [email protected].
Veterans Care Today: Dr Kenneth Campbell Of Tulane University On How The US Has Improved Its Care F was originally published in Authority Magazine on Medium, where people are continuing the conversation by highlighting and responding to this story.